1.3 Bihar
The Indian Government’s launching of the NRHM in 2005 assigned ASHAs an important role as an intermediary between her community and the health system with the goal of improving service delivery and, ultimately, health. ASHAs, like other CHWs, are members of the communities that they provide services to. Generally speaking, ASHAs should be literate women between the ages of 25 and 45 years of age and ideally educated to 10 standard (to about 10th grade). These criteria can be altered in cases where it prevents recruitment.
Bihar is the most rural state in India (Figure 1.1), where most of the livelihood comes from farming activities and most of the population does not live in a strictly urban setting. However, “rural” in this case does not mean sparsely populated, as Bihar has the highest average population density at the state-level in India. Bihar has a population density of just over 1,100 persons/\(km^2\), which is higher than Kerala (at about 860) and higher than any US state (except for Washington DC), and much higher than Finland (39 people/\(km^2\)). For comparison, Bihar and the country of Hungary are fairly similar in size (Bihar is a little larger at 94,000 \(km^2\)), but Hungary has about \(1/10th\) the population of Bihar.
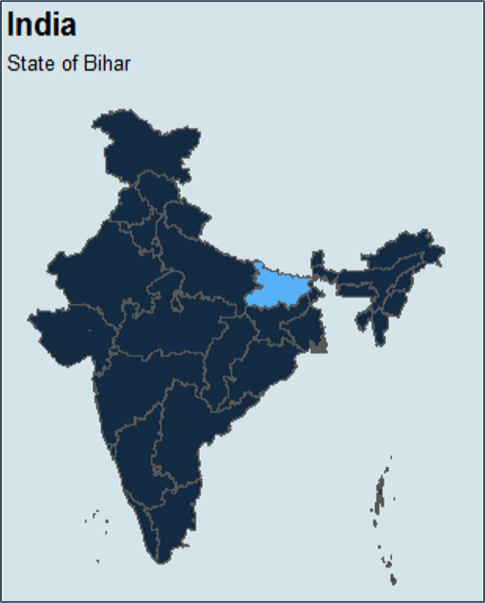
Figure 1.1: Bihar as located within the Country of India
Bihar is the poorest state in India by Gross State Domestic Product, has the country’s lowest expenditure on health, and among the lowest in overall literacy rate (Table 1.1). However, both its population and domestic product are rapidly growing.
| State | Real per capita gross domestic state product | Real per capita revenue expenditure on health | Literacy rate percent year 2013 |
|---|---|---|---|
| Maharashtra | 76,160 | 344 | 84.8 |
| Haryana | 74,337 | 325 | 79.4 |
| Gujarat | 70,906 | 320 | 82.6 |
| Kerala | 66,742 | 591 | 94.8 |
| Uttaranchal | 66,365 | 486 | 82.2 |
| Tamil Nadu | 63,721 | 405 | 82.5 |
| Punjab | 60,405 | 359 | 79.0 |
| Andhra Pradesh | 51,826 | 350 | 70.0 |
| Karnataka | 50,244 | 335 | 78.5 |
| West Bengal | 39,090 | 237 | 79.8 |
| Rajasthan | 35,275 | 301 | 69.2 |
| Chhattisgarh | 35,020 | 269 | 73.0 |
| Odisha | 31,464 | 209 | 76.9 |
| Jharkhand | 31,160 | 176 | 72.5 |
| Madhya Pradesh | 29,913 | 226 | 72.8 |
| Uttar Pradesh | 21,967 | 204 | 74.3 |
| Bihar | 15,557 | 96 | 69.9 |
Many of the health indicators tracked by international development organizations would place Bihar in a zone of concern because it has high levels of infant and maternal mortality. In Table 1.2 one can get an approximate impression of where Bihar is currently (data cerca 2015) with respect to a few of the Millennium Development Goals along with estimates for when these goals might be reached (Prachitha, Dhume, and Subramanian 2019). The overarching desire to see Bihar improve in some of these metrics is a motivator for Project RISE, as is developing a novel and more nuanced perspective on ASHA motivation and performance so that maternal and newborn health can continue to improve. While the indicators in Table (1.2 show improvements from 2005 to 2015, they are nonetheless falling short of the levels of progress hoped for given the concern and level of investment tied to reaching the MGDs. Certainly an even more capable CHW workforce could help in the pursuit of these goals.
| Mdg target | Bihar 2005 | Bihar 2015 | Mdg target value 2015 | Projected year of achieving target |
|---|---|---|---|---|
| Under 5 mortality (per 1000 live births) | 85.0 | 58.0 | 47 | 2021 |
| Infant mortality rate (per 1000 live births) | 61.0 | 42.0 | 25 | 2029 |
| Maternal mortality ratio (per 100,000 live births) | 312.0 | 208.0 | 106 | 2027 |
| Percent of 1-yr-old children immunized for measles | 40.4 | 79.4 | 100 | 2019 |
| Percent of births attended by skilled health personnel | 29.3 | 70.0 | 100 | 2019 |
1.3.1 Bihar Health Care System
Bihar has two interconnected medical systems, government and private. Many people will use both of these systems, augmented by inputs from traditional healthcare experts, family, friends, and other sources. The decision of whether to use government or private medical services is based on the kind of service needed, perception of quality service delivery, distance from the home, cost of service, cost of any bribes needed to access the services, and other factors. In addition to ASHAs, other CHWs include Anganwadi workers (AWWs) and Auxilary Nurse Midwifes (ANMs), all of whom are part of the health system that supports perinatal health initiatives, including providing product- and information-oriented health services (Kosec et al. 2015) such as food supplements and nutritional information, respectively.
Based on the NRHM guidelines, the public, or government, health system in Bihar is organized into three levels (Primary, Secondary and Tertiary levels). To provide integrated curative and preventive healthcare to the rural population, there are Health Sub-Centers (HSCs) and Primary Health Centers (PHCs) at the grassroots (village) and the block level respectively. Sub-centers operate at the village level staffed by auxiliary nurse midwives (ANMs) and assisted by ASHAs. ANMs and ASHAs comprise the outreach services provided under NRHM guidelines and are assigned tasks relating to interpersonal counseling for behavioral change and provide services concerning maternal and child health, family welfare, nutrition, immunization, diarrhea control, and control of communicable diseases programs. Anganwadi Workers (AWWs) are part of the Integrated Child Development Services program (ICDS) primarily focused on nutrition, health, and early learning initiatives.
ASHAs connect pregnant mothers from their communities primarily to the government-regulated health system with duties including: pregnancy registration, providing health information to mothers, administering vaccines, distributing IFA tablets, providing support through regular home visits, and accompanying mothers to the clinic or hospital to give birth. Many CHWs are members of self-help groups (SHGs), which are an increasingly important source of information about health-related norms, cohesion, collectivization, and accountability.
Additional health influencers in Bihar include traditional medical practitioners, religious leaders, and families. Rural medical practitioners (RMPs) are uncertified private health practitioners who have variable backgrounds and levels of expertise. They lack formal accreditation or legal standing as a formal health care practitioner, but often have some biomedical training and may try to align their advice with both traditional medicine and biomedicine. RMPs often run small pharmaceutical shops and may be the health care provider closest to many rural residents.
Dais, also known as Traditional Birth Attendants, have a role similar to a midwife. Dais are the primary health care providers to women during pregnancy and delivery in much of rural India. Their role is largely within the household and despite being local perinatal experts who have apprenticed with an older and more experienced Dai, they are not government certified and do not participate in a government-regulated training program. Most Dais, however, have extensive experience with the birthing process and are well-versed in many health-promoting remedies and practices.
Pandits and Maulvi are, respectively, Hindu and Muslim religious leaders. Many Bihari women seek the advice of religious leaders on a range of topics, and these include customs, rituals, and behaviors surrounding the perinatal period.