12.3 ASHA Positioning
The India Government’s National Rural Health Mission (NRHM) describes the ASHA role as “the interface between the community and the public health system.” Both the focus group discussions and ethnography documented several instances that speak to ASHA as a connector, or as one positioned between systems. We suggest that being a connector of systems, where one is the community where one lives and the other is a formal government system, is an unusual feature of the ASHA’s role that needs more exploration from the perspective of improving performance and motivation.
12.3.1 Positioning Case Study: ASHA and Dai
A somewhat pivotal moment in the synthesis of Project data arrived when we decided to take a closer look at differences in similarities between the ASHA and Dai, particularly with regard to which behaviors they affect and how. This was motivated by two factors, one practical and the other empirical. Practically, across so many observations in multiple data streams, one needs to develop points of entry in order to start to gain some access into a puzzle that it otherwise almost impenetrably complex. Comparing two influencers on certain behaviors is one way to do that. Empirically, we’d noticed that the FGDs and the ethnography both had statements contrasting the role and positioning of the ASHA and Dai in ways that suggested some illuminating relationships could emerge by looking at them more carefully. For instance, results from the FGDs implied that the community respects and trusts the ASHA, but sees the Dais as more “inside the home,” which indicated that some behaviors may be out of reach to the ASHA. In our analogy with a play, this was the first indication that at times ASHAs were simply not on the stage. Similarly, the ethnography observed that in her role as a connector, the ASHA is not seen as part of the household, as the Dai is, nor is she formally a part of a hospital’s medical staff; she is in-between. These observations were the first kernels that lead to thinking about ritual taxonomy and how different behaviors may present greater friction points than others.
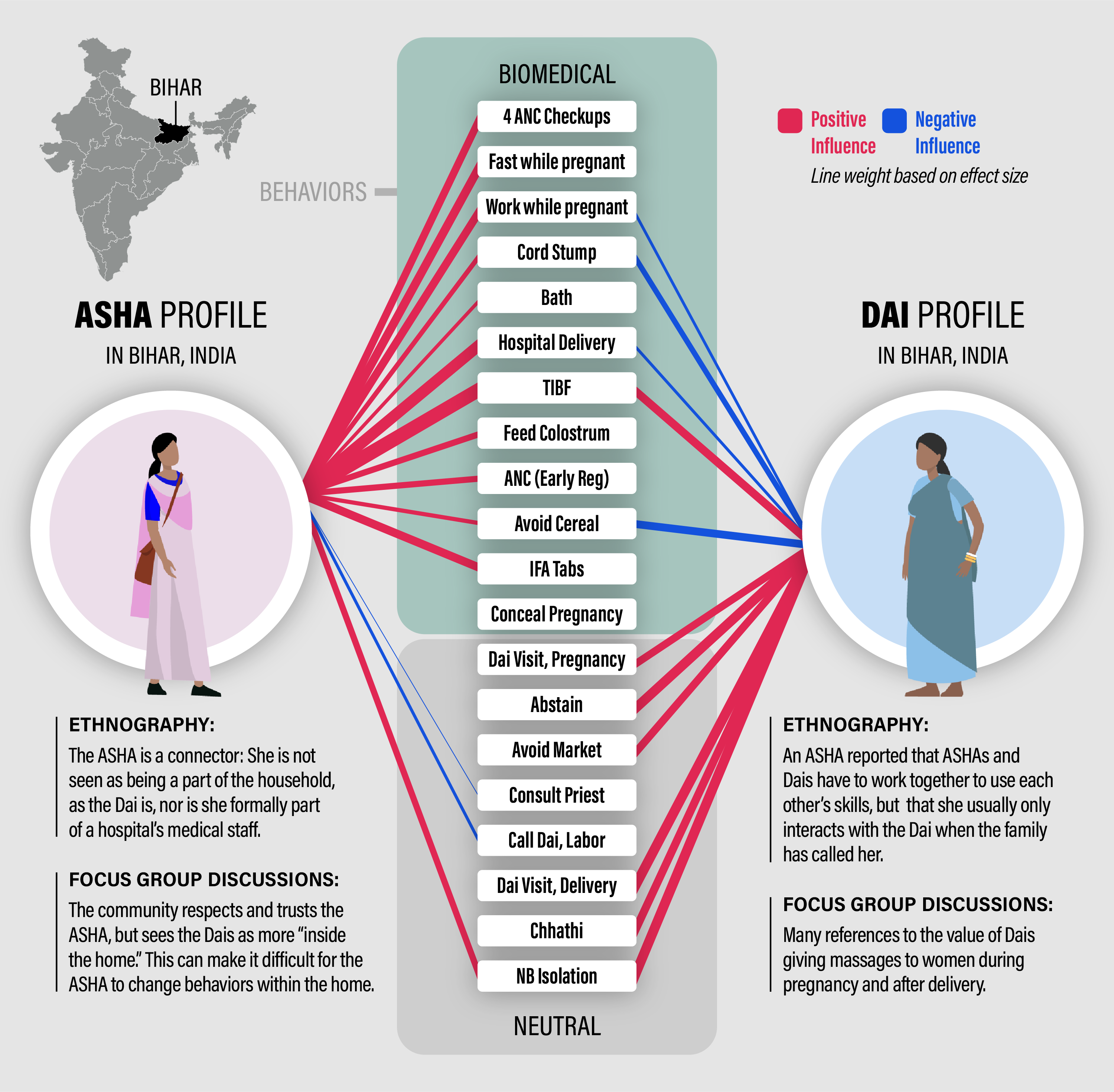
Figure 12.1: ASHA - Dai comparrison: The red lines represent positive effects on the probability that women do the recommended biomedical behavior or do the neutral behavior. Blue lines represent negative effects. The effect is relative to the reference category of no one. The line thicknesses are scaled to the magnitude of the effect. Only effects that have non-overlapping confidence intervals with no one are drawn.
In examining the quantitative data to see if this impression about ASHA - Dai differences would emerge in patterns of influence on behaviors, we weren’t sure what we’d find. However, when examining all of the behaviors together, it became clear that there are important insights to be gained from how Dais and ASHAs differentially impact perinatal behavior (Figure 12.1).
Figure 12.1 contains a lot of information so we’ll try to cover it all carefully. First, the center column is each of the 17 behaviors that are extensively covered in Chapter 8, with the 9 biomedical behaviors on top and the 8 neutral ones below. Importantly, recall that the biomedical behaviors include those that are recommended and not recommended but we model the response as doing what is consistent with biomedical recommendations. That is, a response of ‘yes’ for fasting while pregnant means ‘did not fast’ and a ‘yes’ for concealing the pregnancy means ‘did not conceal’ while a ‘yes’ for hospital delivery means ‘had delivery in hospital.’ The neutral behaviors are not associated with recommendations and hence are just yes for did the behavior or no for did not.
The ASHA is on the left of this column of behaviors and the Dai is on the right. The red lines indicate positive influences on the probability that the response was ‘yes’ relative to the reference category of ‘no one’ (see 8.6 for more information). Blue lines indicate that the influencer lowers the probability that the answer was ‘yes.’ The thickness of the line is scaled for how different the influencer was from no one, so a thicker line means they have a much larger, if red, or much smaller, if blue, effect compared to no one. No one is a useful reference because it is the one option on the influencer part of the survey not directly equated with a specific source of influence. No one is a received normative inclination and when an individual does not readily associate a behavior with an influence she likely selects ‘no one’ as well.
Scanning down the central column from top to bottom, we see that the ASHA has a positive effect on every biomedically recommended behavior and that most of these are not affected by the Dai. When there is not a line drawn from an ASHA or a Dai to a given behavior it means that their effect on the behavior was statistically similar to that of ‘no one.’
In contrast, when we scan down the neutral behaviors, most of which are traditional in nature, we have almost the reverse impression: the Dai positively influences all but one and the ASHA influences very few and more of them negative than positive. Hence, the ASHA’s influence is universally ‘positive,’ inline with biomedical advice, for the biomedical behaviors and absent or spotty for neutral ones.
Moreover, we can look at behaviors that are influenced by both, ASHA and Dai, and place them into two categories: aligned or conflicting.
Aligned behaviors include timely initiation of breastfeeding (TIBF) and mother - newborn postpartum isolation, both of which are behaviors just after delivery. TIBF has been associated with various messaging campaigns and the fact that the Dai is positively associated with it is a good sign. Mother-newborn isolation is coded as ‘neutral’ but there are functional and traditional benefits to this behavior. It helps ensure a clean and safe place for the mother and newborn to rest and recuperate from the birth. It keeps them away from visitors and other inadvertent vectors for bacteria. It includes an assigned family member to act as a primary caretaker.
Contrasting behaviors include working while pregnant (ASHA positive, Dai negative), treating the cord stump (ASHA positive, Dai negative), hospital delivery (ASHA positive, Dai negative), avoiding cereal postpartum (ASHA positive, Dai negative).
Across these connections we see strong support for the impressions gleaned from FGDs and ethnography, that there are some parts of a Mother’s perinatal journey where an ASHA is not really present.
12.3.2 Positioning: Influencers show how ASHA is a connector between systems
The next two figures illustrate the nature of ASHA’s positioning via her influence on (and cognitive association with) a number of behaviors. These quantify her statistical effect, as outlined in Chapter 8. While the figures contain a lot of information, a rather nuanced picture emerges when comparing them.
Figure 12.2 shows ASHA positioning with respect to biomedically impactful behaviors and Figure 12.3 shows ASHA positioning with respect to neutral behaviors. In both cases, the influencers associated with high probabilities of doing the behavior are to the left and with low probabilities of doing the behavior are to the right. An orange box in each row highlights the largest probability for that behavior, hence the strongest positive influencer, and a blue box the lowest probability for the most negative influencer. For the biomedical behaviors in Figure 12.2 we see that the ASHA is always to the left, high influence part of the Figure. She often has the highest positive influence (orange squares) and in that sense is part of the medical system by strength of impact. Sources that we might think of as being closer or more personal to the Mothers are always to the right, toward lower influence of the ASHA. So friends/relatives/neighbors, family, the RMP, the category of ‘no one,’ and the Dai are all mostly the negative or lowest influencers for health behavior.
For the neutral behaviors in Figure 12.3 we see that the ASHA is in the middle, positioned between medical influencers and personal or household influencers, showing her state as a connector. The ASHA has a lowering effect on the probability that Mothers call a Dai for delivery. It is possible that the ASHA and Dai complete a little over this service. Both receive incentives and there has been a large shift in time away from home delivery (Dai’s domain) and toward institutional delivery (ASHA’s domain).
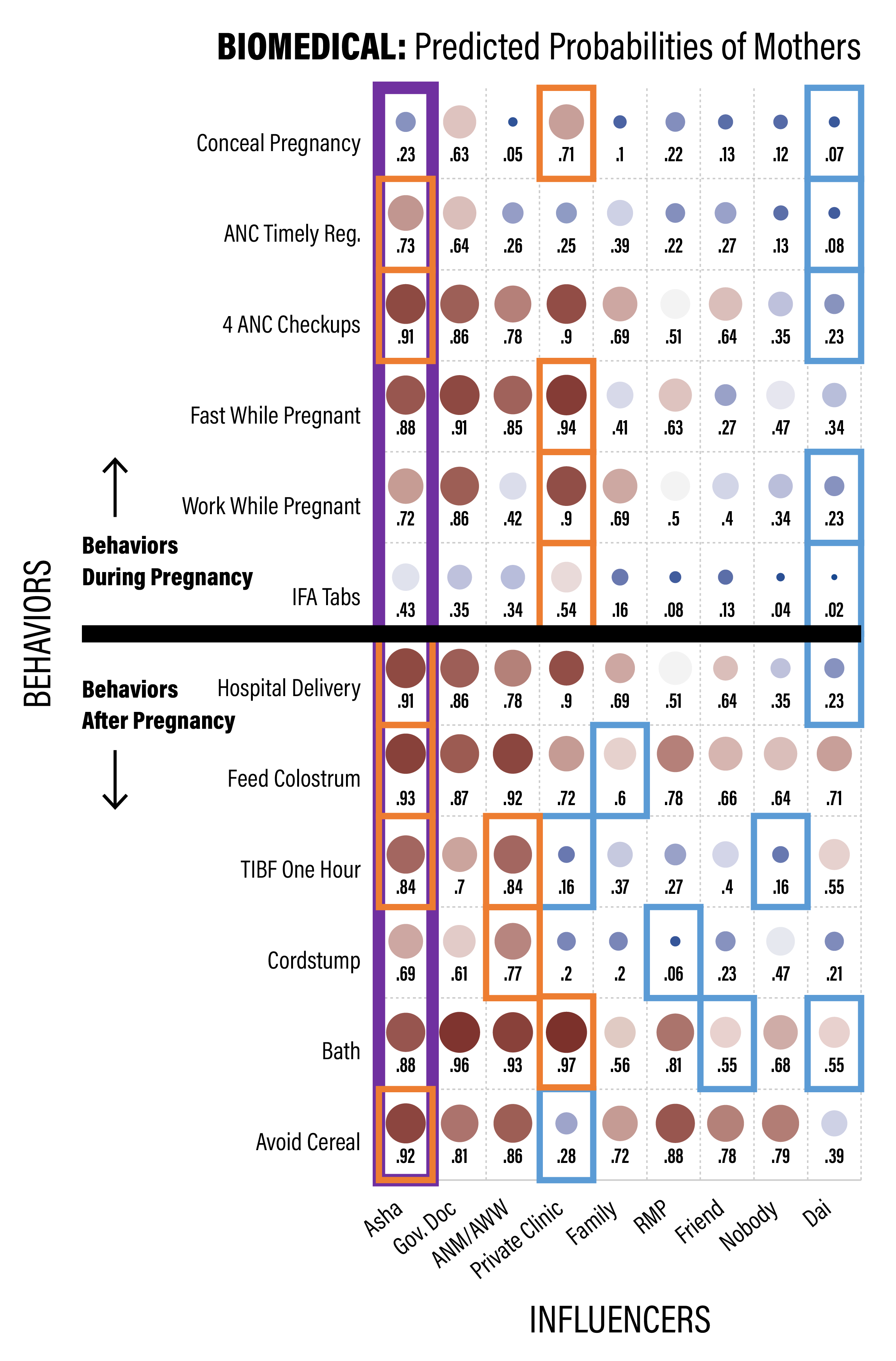
Figure 12.2: ASHA positioning as an influencer of biomedical behaviors for recent mothers. The red squares toward the left are around the largest value for each row, indicating the strongest positive influencer for that behavior, and the blue squares are for the lowest value for each row, indicating the lowest influencer for that behavior.
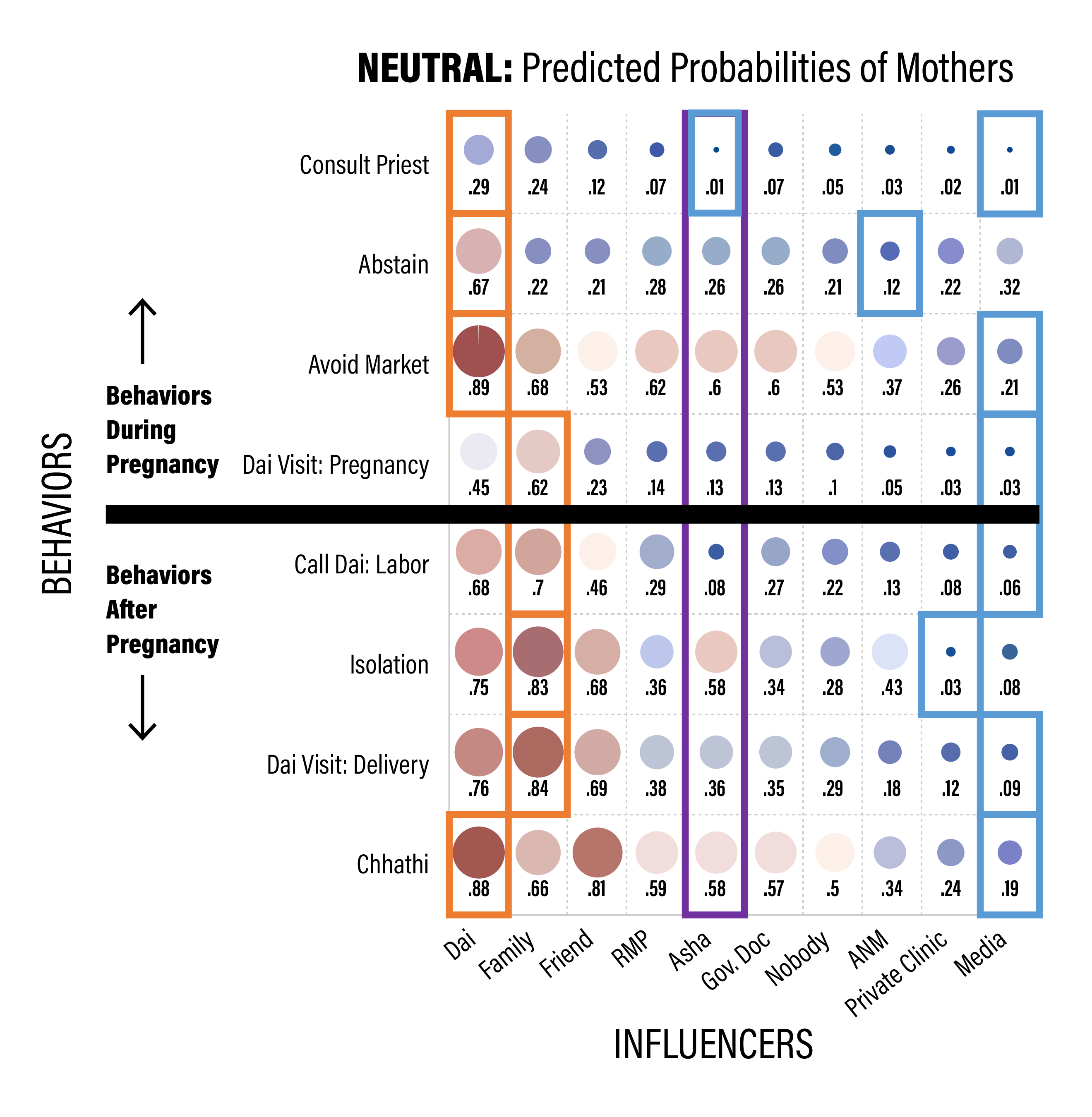
Figure 12.3: ASHA positioning as an influencer of neutral behaviors for recent mothers. The red squares toward the left are around the largest value for each row, indicating the strongest positive influencer for that behavior, and the blue squares are for the lowest value for each row, indicating the lowest influencer for that behavior.