Chapter 6 Reproductive System II
This chapter primarily focuses on the female reproductive system.
6.1 The Ovary
The ovary contains millions of primordial follicles that have been arrested in meiosis I from birth.
Note that ovarian follicles reside in the cortex; the medulla contains major blood vessles and nerves!
6.2 Ovarian follicles
The follicles are made up of oocytes, stroma, and follicular cells (i.e., granulosa and thecal cells).
Granulosa cells are responsible for the generation of the Zona pellucida; thecal cells are specialized connective tissue cells.
During each month, some follicles develop into Graafian follicles (i.e., mature follicles).
6.2.1 Oogenesis
Study the following graphic:
Figure 6.1: Oogenesis
6.3 Ovarian, Menstrual, and Uterine Cycle
6.3.1 Menstrual cycle
This occurs during the onset of puberty to a female’s menopause; while cycle lengths do vary, it takes an average of 28 days for one cycle of the menstrual cycle to be completed.
Vaginal bleeding is the most common feature of the menstrual cycle and involves two cyclic changes:
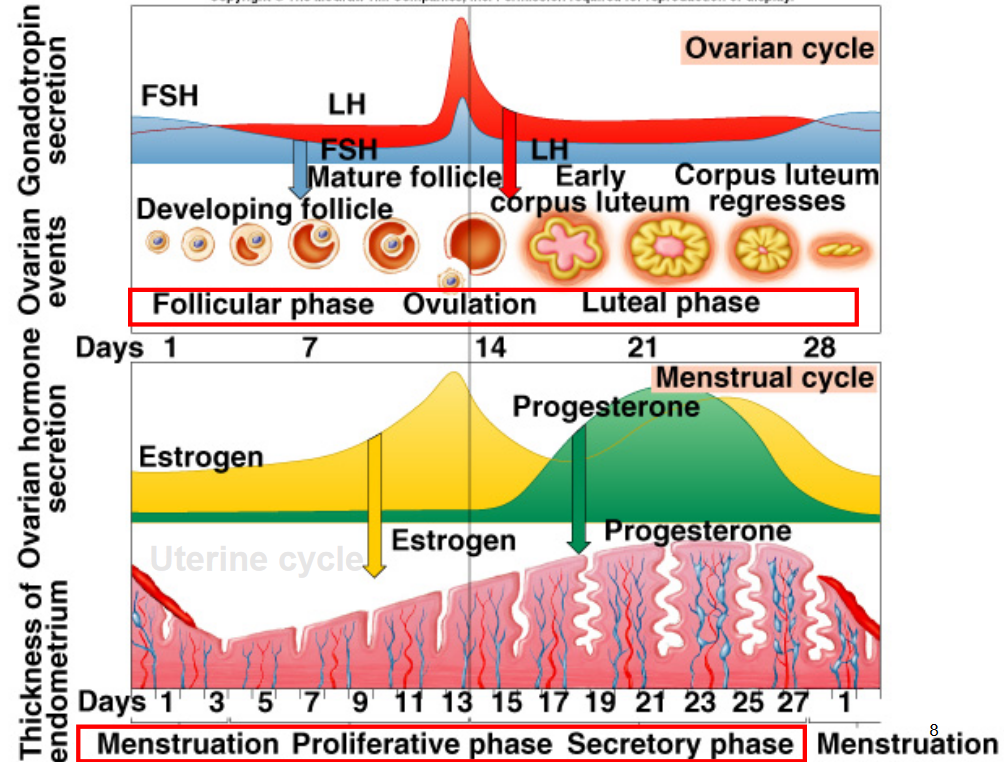
Figure 6.2: Hormone Levels in the Menstrual Cycle
6.3.1.1 Disruption of the menstrual cycle
Disruptions can be caused by many factors: abnormalities in the hypothalamus - pituitary - ovary axis, low body weight, improper diet, and vigorous physical activity to name a few.
Amenorrhea refers to the absence of menstruation ; oligomenorrhea refers to irregular intervals of menstruation.
While improper menstruation has been linked to poor bone health (due to the lack of estrogen secretions), it may also lead to lower cancer risks.
Note that the menopause is the cessation of the menstrual cycle.
6.3.1.2 Contraceptives
The pill is made up of synthetic estrogen or progesterone. This is in contrast to the minipill - only progesterone is present.
One should also note that the pill has cardiovascular side effects (e.g., increased blood clotting); though, whether or not the pill increases cancer risks is still up for debate.
The morning after pills Plan-B and Ella uses RU846 - a progesterone receptor antagonist.
6.3.2 Ovarian cycle
6.3.2.1 Days 1 - 13 (follicular phase)
There is oocyte growth; thecal cell proliferation and granulosa cell growth also takes place here.
6.3.2.1.1 Hormonal regulations of the follicular phase
The hormones LH and FSH stimulate estrogen synthesis; estrogen and FSH stimulate granulosa cell proliferation and follicle maturation.
Moderate levels of estrogen inhibit the production of estrogen, FSH, and LH; FSH-producing cells are more sensitive to estrogen,
6.3.2.2 Day 14 (ovulation)
The enlarged, mature follicle is on the surface of the ovary - the secondary oocyte is expelled.
6.3.2.2.1 Hormonal regulations during ovulation
A high amount of estrogen actually encourages causes a massive, abrupt surge in LH secretions.
Ovulation is triggered by producing prostaglandins and activating proteases through progesterone receptors.
Figure 6.3: Ovulation Triggering
6.3.2.3 Days 15 - 28 (luteal phase)
Follicular cells are first converted into steroidogenic cells that are responsible for forming the corpus luteum.
A large amount of progesterone and a moderate amount of estrogen are secreted to prepare for the implantation of the fertilized egg.
6.3.2.3.1 Hormonal regulations of the luteal phase
As mentioned previously, LH triggers the differentiation of follicular cells into luteal cells and stimulates the secretion of a large amount of progesterone (and a smaller amount of estrogen).
Both progesterone and estrogen inhibit LH and FSH secretions. When the corpus luteum finally degenerates, this allows for the moderate secretion of LH and FSH, hence causing the next ovarian cycle to happen.
6.3.3 Uterine cycle
6.3.3.1 Structure of the uterus
Figure 6.4: Layers of the Uterus
The endometrium is comprised of stratified epithelium, stroma, and glands.
The myometrium is made up of smooth muscle
The perimetrium is made up of simple squamous epithelium and connective tissue.
6.3.3.2 Phases of the uterine cycle
6.3.3.2.1 Proliferative phase (the follicular phase)
Here, estrogen stimulates the growth of epithelial cells and blood vessels.
6.3.3.2.2 Secretory phase (the luteal phase)
Progesterone converts the thickened epithelium (from the proliferative phase) into highly vascularized, glycogen-filled tissue.
6.3.3.2.3 Menstrual phase (end of the luteal phase)
The endometrium necrotizes and sloughs away (i.e., period blood) - the corpus luteum also degenerates.
6.4 Fertilization
This happens in the ampulla:
Figure 6.5: Fertilization in the Ampulla
The hyaluronidase in the sperm’s acrosome carves a channel through the zona pellucida, hence allowing the sperm cell to fuse with the ovum’s cell membrane
The ovum membrane then disappears and a zygote is formed.
6.4.1 Implantation
The zygote (i.e., the fertilized egg) divides through the fallopian tube - on the sixth day of fertilization, the blastocyst then attaches to the uterine wall.
Trophoblastic cells first develop into the fetal position of the placenta, and the inner cell mass differentiates into the fetus.
Thereafter, trophoblast cells begin to secrete hCG after implantation - hCG also exerts LH-like effects to maintain the corpus luteum. The presence of hCG can be detected in a pregnancy test.
6.4.2 Placenta
Observe the structure of the placenta:
Figure 6.6: Formation of the Placenta
6.5 Hormones
6.5.1 Estrogen
This hormone:
- Stimulates endometrial growth
- Inhibits prolactin secretions
- Stimulates the growth of mammary ducts
- Promotes bone and cardiovascular health
6.5.2 Progesterone
This hormone:
- Inhibits endometrial growth (induced by estrogen)
- Suppresses uterine contractions (by forming mucous plugs)
- Stimulates gland secretion and the development of mammary ducts.
6.5.3 Placental lactogen
This is the so-called growth hormone of pregnancy - the amount of placental lactogen secreted is proportional to the size of the placenta.
Placental lactogen is structurally similar to the growth hormone and prolactin - it also encourages lipolysis and reduced glucose utilization.
Placental lactogen also prepares the mammary gland for lactation.
6.6 Mammary Glands
A mammary gland consists of mammary ducts and alveoli - the alveolus is the functional structure of the breast.
Clusters of alveoli are called lobules - lobules form lobes.
6.6.1 Mammary development in mice and rats
While there are a few rudimentary mammary ducts are present at birth, it is limited to mammary ducts and buds before puberty (though there are alveoli in mature animals).
There is also extensive ductal and alveoli development during pregnancy - after weaning, the glands undergo involution and many mammary cells undergo apoptosis (i.e., cell death).
6.6.2 Estrogen and progesterone receptors
ER\(\alpha\) mediated estrogen action is essential for ductal morphogenesis. PR-mediated progesterone action, on the contrary, is required for ductal branching and alveoli development.
6.6.3 Lactation
Figure 6.7: Lactation
During lactogenesis I, there is cytological and enzymatic differentiation of alveolar cells before parturition. There is an increase in the amount of endoplasmic reticulum, an increase in enzymes, and limited milk synthesis and secretion.
During lactogenesis II, there is the onset of milk secretion. This occurs in women 1 - 2 days postpartum.
Lactogenesis III refers to the maintenance of milk secretion.