Chapter 7 Digestive System
Shown are the anatomical structures of the digestive system:
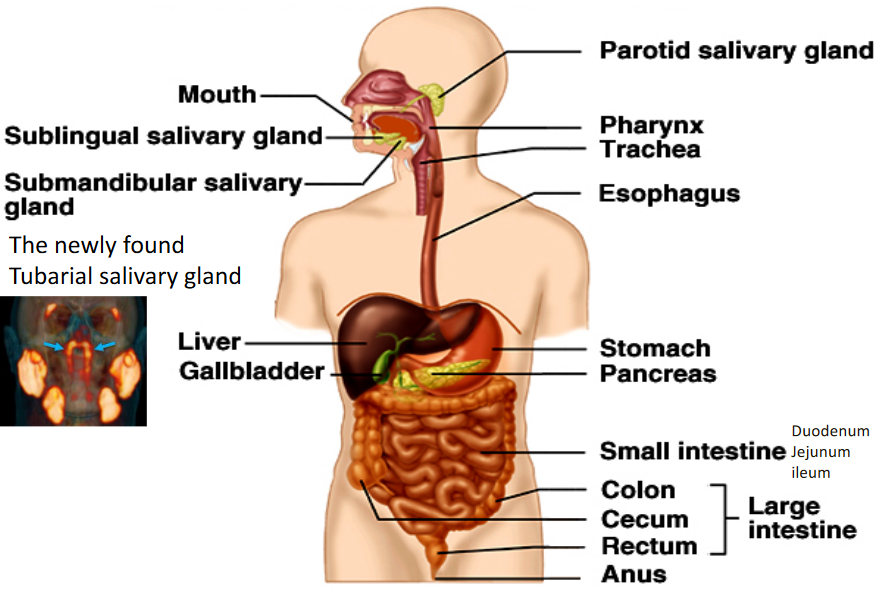
Figure 7.1: Anatomy of the Digestive System
7.1 Anatomy of the Digestive System
The GI tract has four different layers: the mucosa, the submucosa, the muscle layer, and the serosa.
The mucosa has three different layers:
- A layer of simple columnar epithelium lining the lumen
- A thin layer of connective tissue
- A thin layer of smooth muscle
The submucosa is comprised of loose connective tissue with blood vessels, lymphatic vessels, and nerves.
The muscularis has an inner layer of smooth muscle and an outer, longtiduinal layer of smooth muscle.
The serosa is made up of connective tissue with simple squamous epithelium.
Figure 7.2: Layers of the GI Tract
7.2 Regulations and Functions of the Digestive System
7.2.1 Functions
The digestive system performs a variety of different functions:
It moves food through the intestines via a combination of peristalsis (i.e., propulsive movement) and segmentation (i.e., mixing movement).
The digestive system also secretes the following hormones (alongside other hormones from endo- and exocrine glands).
Lastly, the digestive system also digests food via degrading ingested food into monomeric units. Absorption of these “monomeric units” also take place in the small and large intestine.
7.2.2 Regulations
7.2.2.1 Smooth muscle contractions
Smooth muscle in the gastrointestinal tract have a basic electrical rhythm due to Interstitial Cells of Cajal (i.e., “pacemaker” cells) that generate a basic electrical rhythm.
When a “depolarization threshold” is reached, an action potential happens and spreads to the surround smooth muscle tissue via the functional syncytium through gap junctions. This induces smooth muscle contractions and hence, peristalsis and / or segmentation.
The activity of these interstitial cells are regulated by hormonal and nervous factors.
Figure 7.3: Action Potential Graph of Interstitial Cells of Cajal
7.2.2.1.1 What is the functional syncytium?
It is a group of smooth muscle cells connected by gap junctions that electrically and mechanically function as a unit.
These units are found in urinary, digestive, and reproductive tracts; as mentioned previously, an action potential from the interstitial cells of cajal quickly spread to other cells via functional syncytiums.
Figure 7.4: A Functional Syncytium
7.2.2.2 Intrinsic nerve plexuses
This is also known as the enteric nervous system (the system has ~100 million neurons in total). All three types of neurons: sensory, motor, and interneurons are present here, and the plexus is made up of submucosal and myenteric plexuses.
Submucosal plexuses are able to sense the environment via the lumen and regulate gastrointestinal blood flow and gland secretions.
Myenteric plexuses control the mobility of food (through the gastrointestinal tract).
Figure 7.5: Myenteric and Submucosal Plexuses
7.2.2.3 Extrinsic nerves (sympathetic and parasympathetic)
Extrinsic nerves contain a synapse (i.e., a gap between two neurons) and an intrinsic nerve plexus; these nerves act directly on smooth muscle and glands.
Parasympathetic activation of these nerves stimulates gastrointestinal secretions and mobility of food. The vagus nerve innervates the tract from the esophagus to the traverse colon (i.e., the part of the large intestine moving across the body). The pelvic nerve descends from the colon to the anus.
Sympathetic activation, on the contrary, inhibits gastrointestinal secretions, reduces food mobility, and causes vasoconstriction.
7.2.2.4 Gastrointestinal hormones
Gastrin is secreted by the G cells of the stomach. Not only does it encourage secretions from the parietal cells (secretes HCl) and chief cells (secretes pepsinogen) of the stomach, but it also relaxes the pyloric sphincter (prevents food from travelling from the stomach to the duodenum - the first part of the small intestine) and encourages the movement of food through the gastrointestinal tract.
Secretin is released in response to acid being in the duodenum. This hormone encourages NaHCO3 secretion by the pancreas and the liver.
Cholecystokinin stimulates the pancreatic secretion of digestive enzymes and promotes the relaxation of the gallbladder and the sphincter of Oddi.
Gastric inhibitory peptide (i.e., GIP) stimulates insulin production.
It is important to note that secretin, cholescystokinin, and GIP inhibits gastric emptying and secretions!
Figure 7.6: Regulation of the Digestive System
7.3 The Stomach
This is the most distensible part of the gastrointestinal tract; gastric pits are “trenches” in the epithelial lining of the stomach:
Figure 7.7: Anatomy of the Stomach
7.3.1 Gastric secretions
As mentioned in the previous sub-chapter, parietal cells secrete HCl, but they also secrete intrinsic factors. HCl serves to kill bacteria, denature proteins, and also activate pepsinogen to pepsin.
Enterochromaffin-like cells make histamines.
Chief cells secrete pepsinogen.
Mucous cells secrete alkaline mucous. Mucous is important to prevent the stomach from digesting itself.
G cells make gastrin.
There are three phases for regulating gastric secretions:
Figure 7.8: Regulating Gastric Secretions
Furthermore, D cells also regulate the production of HCl in parietal cells:
Figure 7.9: Regulating HCl Secretions
7.3.3 Regulating gastric motility
An increased amount of chyme (digested food that has been mashed up into a milkshake-like consistency) and chyme fluidity encourages gastric emptying.
Several duodenal factors also delay gastric emptying:
- Fats (the most potent factor)
- Acids (inside the duodenum)
- Hypertonicity (i.e. a hypertonic environment)
- Distensity (i.e., when the stomach is stretched full of food)
Neural factors also regulate gastric motility. These include intrinsic nerve plexuses, vagus nerve stimulations, and emotions (i.e., angry individuals have better gastric emptying than depressed individuals).
Hormonal factors too play a role. The hormones gastrin, secretin, cholecystokinin, and GIP from the duodenum inhibit it.
7.3.3.1 Gastroparesis
This is a condition characterized by delayed gastric emptying; this condition can also be caused by a damaged vagus nerve.
A third of all diabetic patients have this condition.
7.3.4 Vomiting and the control of vomiting
Vomiting is due to the activation of the vomiting center in the medulla.
When a person vomits, their diaphragm (a dome shaped muscle under the lungs responsible for generating negative pressure) and abdominal muscle contracts, and their esophagus and gastroesophageal sphincters relax.
Because of the acidic and watery contents of the gastrointestinal tract, vomiting has the potential to cause dehydration and in some cases, metabolic alkalosis.
7.4 The Pancreas
Figure 7.10: Anatomy of the Pancreas
7.4.1 Pancreatic secretions
Sodium bicarbonate (i.e., NaHCO3-) neutalize the acidity of chyme.
Zymogens are secreted proteolytic enzymes; these include:
- Trypsinogen (activated by enterokinase to trypsin)
- Chymotrypsinogen to chymotrypsin
- Procarboxypeptidase to carboxipeptidase
Amylase digests polysaccharides (e.g., starch) to maltose.
Lipase - the only enzyme in the gastrointestinal tract - digests fat by hydrolyzing triglycerides to monoglycerides and fatty acids. A deficiency of this enzyme can result in a condition called Steatorrhoea (i.e., “fatty” diarrhea - stool secretions are black / pale-looking and foul-smelling).
7.5 The Liver
The liver has a broad range of functions:
The liver processes nutrients, produces bile for digestion, and degrades and detoxifies hormones, body wastes, and pharmacological agents (i.e., over-the-counter medications).
Furthermore, the liver also synthesizes plasma proteins and clotting factors (not including immunoglobins), store fats, iron, copper, vitamins, and glycogen, and activates vitamin D and the thyroid hormone.
Kupffer cells in the liver also removes worn-out red blood cells.
7.5.1 Blood Circulation in the Liver
There are two major blood vessels in the liver: the hepatic portal vein and the hepatic portal artery.
The portal vein delivers digested substances from the stomach to the liver.
The portal artery delivers O2 and nutrients from the heart.
The hepatic vein returns blood from the liver to the heart (to be oxygenated again).
7.5.2 Hepatic lobules (the functional unit of the liver)
Observe the general anatomy of a hepatic lobule:
Figure 7.11: Hepatic Lobule Anatomy
Interestingly, the liver seems to have an infinite capacity for regenerating itself. 90% of liver cells (i.e., hepatocytes) are replaced within a day of the injury.
However, the liver does not heal very well when it is scarred (caused by a condition known as cirrhosis - the scarring and hardening of the liver).
7.5.3 Bile production in the liver
Bile contains bile salts, cholesterol, lecithin, bilirubin, and NaHCO3-. The bile duct opens up to the duodenum and its opening is guarded by the sphincter of Oddi which closes between meals. The gallbladder store bile.
Cholecystokinin stimulates gallbladder contractions and the relaxation of the sphincter of Oddi to deliver bile into the gut.
7.5.4 Bile salts
These are amphipathic substances that emulsify lipids to increase the surface area of fat. Bile salts also solubilize lipids.
Bile salts are responsible for the majority of cholesterol digestion in the body:
Figure 7.12: General Structure of a Bile Salt
Up to 95% of bile salts end up back in the liver for re-secretion!
7.5.4.1 Regulating bile salt secretions
Secretin stimulates the release of aqueous NaHCO3-
The vagus nerve also plays a role in stimulating bile salt secretions.
7.5.5 Gallstones
Cholesterol stones account for 90% of all gallstones. These stones can be caused by the hypersecretion of cholsterol, the hyposecretion of bile salts, and a malfunctioning gallbladder.
Pigment stones account for 10% of all gallstones; they are made up of a large amount of bile pigments (e.g., billirubin) and lesser amounts of cholesterol and calcium salts.
7.6 The Small Intestine
The small intestine includes the duodenum, jejunum, and the ileum. It is also the site where the bulk of digestion and absorption takes place.
The inner surface of the small intestine also contains many folds to increase the amount of surface area of digestion: villi increase the surface area by an order of 10; microvilli arise from the brush borders of epithelial cells and increases the surface area by another 20 times.
7.6.1 Enzymes in the small intestine
Enzymes here are contained in brush borders - these enzymes have their active sites exposed to the lumen.
The main enzymes in the small intestine are:
- Enterokinase
- Aminopeptidase
- Maltose, sucrase, and lactose
Figure 7.13: Blood Supply to the Small Intestine
7.7 The Large Intestine
Absorption of water and electrolytes take place here.
Microbial fermentation (i.e., digestion of cellulose) and vitamin K and biotin synthesis can also occur here.
The large intestine is also where feces (i.e., poop) is made.
7.7.1 Defecation Reflex
When the rectum (where feces are stored) is stretched, this stimulates defecation. The muscularis (third layer of the gastrointestinal tract) contracts and the internal sphincter relaxes - defecation can only occur when this happens!
The myenteric plexus can also cause defecation!
Figure 7.14: Rectum and Anal Canal Anatomy