Chapter 5 Reproductive System I
Observe the structure of the reproductive system in a human male and female:
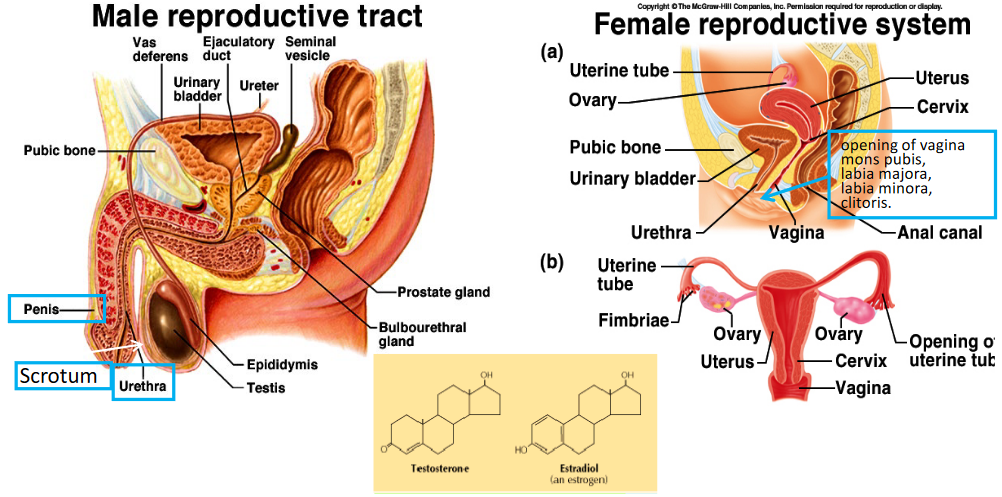
Figure 5.1: Male and Female Reproductive System
Note that the parts highlighted in blue are key structures to know - also note the sex hormones testosterone and estradiol that are necessary for proper sexual development.
5.1 What is “Sex?”
The idea of “sex” can be defined at three levels:
- Genetic sex
- Gonadal sex
- Phenotypic sex
Figure 5.2: Three Levels of Sex
5.1.1 Relationship between genetic and gonadal sex
In the case of males, the SRY gene (i.e., Sex-Determining Region of the Y) encodes for the SRY protein (i.e., the testes-determining factor [TDF]); the latter protein then encodes for the SOX9 protein, hence causing the primitive gonads to differentiate into testes.
5.1.1.1 What is SOX9?
SOX9 is a direct target of the SRY gene:
Figure 5.3: SOX9 Protein in Mice
A mutation in the SOX9 protein causes male to female sex reversal in human and mice. The SOX9 induces testes development and male behavior in XX human and transgenic mice.
5.1.1.2 DAX1
DAX1 is normally expressed in primitive gonads, but down-regulated in males.
XY males carrying extra copies of DAX1 showed delayed testes development; sex reversal happens when the transgene is tested against the weak alleles of SRY (DAX1 inhibits the SF1 induced activation of SOX9).
Duplication of the DAX1 gene in a XY male leads to male-female sex reversal
5.1.1.3 SRY-RSPO1 is critical for ovary development
A family of four XX brothers who had no insertion of SRY gene, but a loss of function mutation in RSPO1.
Furthermore, there is also a 46XY individual who had duplicated regions of chromosome 1 that contained RSPO1 - this caused male-to-female sex reversal. Similar sex reversals were observed in transgenic mice.
Figure 5.4: RSPO1 Mechanism
R spondin develops the ovaries via signalling of beta-catenin.
5.1.1.4 In short…
Here is a short summary of what has been discussed thus far:
Figure 5.5: Summary of Sex Determination
5.1.2 Disorders of chromosal sex
There are a couple of disorders that can result chromosomal aneuploidy:
5.1.2.1 Turner’s syndrome
There is a \(\frac{1}{2500}\) chance that a female will end up with this. Patients only have one X chromosome.
5.1.2.2 Triple X syndrome
There is a \(\frac{1}{1000}\) chance that a female will end up with this. Patients have three X chromsomes.
5.1.2.3 Klinefelter syndrome
There is at least one X chromosome in males (i.e., the genotype is XnY, where “n” is at least two).
5.1.2.4 Jacobs syndrome
The genotype of the affected male is XYY; this happens to \(\frac{1}{1000}\) male births - 96% of all sufferers are phenotypically normal.
5.1.2.5 Disorders due to endocrine disorder
A defect in androgen receptors results in the developmental failure of the male reproductive system (e.g., failure to secrete androgens or a defect in the androgen receptor gene).
A genetic deficiency of 5-\(\alpha\)-reductase results in the failure of the development of the male reproductive tract. Adrenal androgen hypersecretion may also cause genital ambiguity in female infants.
5.2 Male Reproductive System
Observe the components of the male reproductive system:
Figure 5.6: Male Reproductive System
Seminal vesicles provide the bulk of the semen (60%). Its main function is to secrete fructose to nourish sperm, secretes prostaglandins to stimulate smooth muscle contractions, and secrete fibrinogen to clot the semen.
The prostate gland secretes alkaline fluid (30% of semen) to neutalize vaginal acids, provides clotting enzymes to clot the semen, and fibrinolysin to degrade the “clot.”
Bulbourethral glands secrete mucous for lubrication.
5.3 Histology and function of testes
Seminiferous tubules contains germinal cells and sertoli cells. Spermatogenesis also happens here.
Figure 5.7: Leydig Cells
Leydig cells are responsible for secreting testosterone.
5.3.1 Sertoli cells
These cells form tight junctions to form the testes-blood barrier, produces chemicals and proteins to nourish spermatogenic cells, and establish the stem cell niche to ensure renewal of sperm cell precursors.
Androgen-binding protein (i.e., ABP) - which binds to testosterone to concentrate the hormone in the tubules - is also produced here. Inhibilin (inhibits FSH release) and AMH are also produced.
Also, note the following graphic (note that spermatogenesis is essential for both mitosis and meiosis):
Figure 5.8: Spermatogenesis
5.3.2 Structure of a spermatozoan
The head of the spermatozoan contains the nucleus; the acrosome contains enzymes (hyaluronidase) for penetrating the zona pellucidum of the egg. The midpiece contains a large amount of mitochondria to power movement; the tail is responsible for movement.
5.4 Androgens
These include adrenal and testicular androgens; testosterone is secreted by the Leydig cells.
Testosterone is converted into dihydrotestosterone by 5-\(\alpha\)-reductase in some tissues (e.g., bone, brain, muscle, testes, kidney, etc).
5.4.1 What do androgens do?
Androgens promote the descending of the testes into the scrotum; they also induce the development of male genitalia.
Furthermore, androgens are responsible for growing and maturing the reproductive system: it also maintains the function of the male reproductive system and induces male-pattern behavior.
Androgens can also promote bone growth and protein anabolism:
Figure 5.9: Regulation of Hormones in the Male Reproductive System
5.5 Anabolic steroids
These are synthetic compounds whose functions are similar to testosterone and targets androgen receptors.
While anabolic steorids are generally used in hormone therapy, they are also abused.
Consequently, anabolic steroids can cause the following short term effects in males:
- Baldness
- Impotence
- Testicular atrophy
In females, the following short term effects can result:
- Irreversible masculine features
- Uterine atrophy
- Mestrual iregularities
Long term usage of anabolic steroids can lead to aggression, cardiac disease, hostility, and an increased risk of liver cancer!.
5.6 What are Prostaglandins?
These are chemical messengers that are virtually found in all tissues. They are 20-carbon fatty acid derivatives from arachidonic acid and act locally and are rapidly inactivated after action.
Furthermore, letter designations (e.g., PGA, PGE, PGF) denote structural variations in the five carbon ring:
Figure 5.10: Some Prostaglandins
Note that the number designations (e.g., PGE1, PGE2, etc.) denotes the number of double bond in the side chains.
Prostaglandins are synthesized via the following graphic:
Figure 5.11: Prostaglandin Synthesis by Cyclooxygenases
Note that prostaglandins have very broad functions (e.g., reproduction and ovulation).