Chapter 2 Introduction to Physiology
Physiology arose all the way back from 470 BC, when the Greek philosophers Socrates (470 - 399 BC) and Aristotle (384 - 322 BC) discovered heart rates in developing chicken embryos.
Thereafter, William Harvey (1578 - 1657) figured out how the human heart operated; for this reason, Harvey is often referred to as the founding father of modern physiology.
In the 19th century, Claude Bernard (1813 - 1867) and Walter Cannon (1871 - 1945) coined the idea of homeostasis.
There is no need to memorize any part of the below figure; it merely serves to give the reader a bird’s eye view of past, important scientific discoveries:
Figure 2.1: Some Past, Important Events in Science
If anything, it is important to realize that Physiology is an integrative science!
2.1 Cell Types and Body Organization
Cells are the smallest, living entity and the “building blocks” of the body
Tissues, on the other hand, are comprised of cells that are similar in structure and function. There are four main types of tissues examined in BS2001:
- Epithelial
- Connective
- Muscle
- Nervous
Organs are structures that are made up of at least two different types of tissues (e.g., the skin is made up of epithelial and adipose tissue). Each tissue in an organ serves a different purpose.
Lastly, an organ system is located in various regions of the body; organs that are part of a system perform related functions (e.g., veins and arteries serve to bring oxygenated, nutrient-rich blood to tissues from the aorta and carry deoxygenated, nutrient-poor away from tissues back to the heart).
2.1.1 Epithelial tissues
Epithelial tissues can be come in three different shapes and serve a variety of purposes:
Figure 2.2: Types of Epithelial Tissue
Squamous epithelium (flat with a raised center, like a ravioli) are generally used for diffusion and filtration purposes. They line the oral cavity (i.e., the mouth), the pulmonary aveoli (i.e., tiny air sacs in your lungs), and the glomerulus of your kidney.
Cuboidal (cube-shaped) epithelium serve excretion, absorption, and secretion purposes. They line salivary ducts, pancreatic ducts, and also kidney tubules.
Columnal (like a column) epithelium also serve the same function as cuboidal epithelium, albeit they are found in the digestive tract (i.e., the walls of the small intestine) and uterterine tubes.
Furthermore, simple epithelial tissue are one cell-layer thick and are typically used for transport purposes. Stratified epithelium come in multiple cell layers and are designed for protection purposes.
2.1.1.1 Some other things to note about epithelial tissue
First and foremost, epithelial tissue is avascular.
The basement membrane of epithelial tissues contain the following compounds, all of which are secreted by epithelial cells:
- Collagen
- Laminin
- Glycoproteins
- Proteoglycans
Mnemonic: CLGP
The reticular laminar, on the contrary, has collagen fibers that are secreted by fibroblasts.

Figure 2.3: The Basement Membrane
Lastly, there are three sides to epithelial tissue:
The apical surface is the topmost layer.
The basal surface is connected to the basement membrane.
The lateral surface has tight, adherens, and gap junctions.
2.1.2 Connective tissue
There are two types of connective tissue:
Dense connective tissue have a high amount of collagen fibers, but a lesser amount of connective tissue cells. Such connective tissue can be further sub-divided into two categories: regular and irregular:
Figure 2.4: Types of Dense Connective Tissue
This is in contrast to loose connective tissue: such connective tissue have a lower amount of collagen fibers, but a higher amount of connective tissue cells:
Figure 2.5: Loose Connective Tissue
NB: blood, bone, and cartilage are ALL special types of connective tissue!
2.1.2.1 Connective tissue cells
Fibroblasts are the most common connective tissue cells.
This is followed by adipocytes, macrophages, plasma cells, and mast cells (which produce histamines and heparin).
2.1.2.2 Connective tissue matrix
There are several protein fibers that comprise the matrix:
- Collagen serves to make the matrix strong, yet flexible.
- Elastin makes the matrix stretchy and elastic.
- Reticulin - thin collagen fibers with glycoproteins - are also present.
There are also a variety of large and small ground molecules (e.g., electrolytes, nutrients, etc.) and water molecules that are included in the matrix.
2.1.2.3 Functions of connective tissue
Obviously, connective tissue serves to connect cells and organs together (e.g., connecting skin to muscle).
However, connective tissue also provide strong, flexible support and elasticity to tissues (e.g., elastin fibers in the lungs).
Connective tissue can also fill up spaces, store fat, and provide cushion (e.g., the eye is cushioned by adipose tissue).
Lastly, connective tissue is also a site for immune response and plays a variety of other roles too, including but not limited to wound healing, tissue remodelling, and immune response.
2.1.3 Muscle tissue
Study and know the following graphic:
Figure 2.6: Types of Muscle Tissue by Structure
Skeletal muscle cells are striated with multiple nuclei.
Cardiac muscle are branched, striated, and fused at their plasma membranes.
Lastly, smooth muscles are thin and wispy, have one nucleus, and found in internal, hollow organs.
2.1.4 Neural tissue
A nerve cell has three components: a dendrite, a cell body, and an axon. Its main purpose is to generate and transmit electrical signals.
There are also supporting cells (there are many supporting cells, but the ones examined in BS2002 are shown below):
Astrocytes physically support neurons and are responsible for the formation of the blood-brain barrier.
Schwann cells and oligodendrocytes are responsible for generating the myelin sheath of the peripheral and central nervous system.
Microglia function as the central nervous system’s so-called “immune” cells.
Ependymal cells line the internal cavities of the brain and the spinal cord.
2.1.4.1 Neural regulation basics
Study and remember the following graphic:
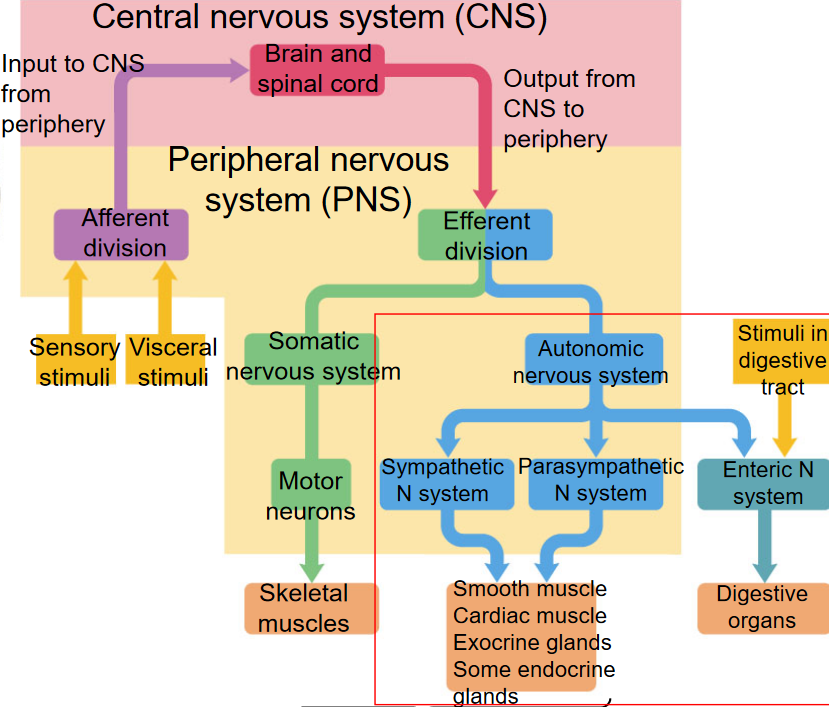
Figure 2.7: Neural Regulation Pathway
There are also three major classes of neurons: afferent (carries signals away from the receptor), efferent neurons (carries signals towards the effector), and interneurons (between afferent and efferent neurons):
Figure 2.8: Types of Neurons
Nevertheless, neurons are excitable: they have a threshold potential. When the threshold potential is reached, this will result in a change in their membrane permeability, ultimately resulting in an action potential:
Figure 2.9: How Action Potentials Work
The action potential is conducted along the nerve as one, long electrical impulse.
Figure 2.10: Membrane Potentials
Furthermore, neurotransmitters relay information between neurons:
Figure 2.11: Acetycholine as a Neurotransmitter
Yet, it is important to note that there are different neurotransmitters for different autonomic nerves:
For the parasympathetic pathway, acetycholine is both the pre-ganglionic, nicotinic and post-ganglionic, muscarinic (a ganglion is a bundle of nerve cells) neurotransmitter.
For the sympathetic pathway, acetycholine is a nicotinic, pre-ganglionic neurotransmitter, and norepinephrine is an adrenergic, post-ganglionic neurotransmitter.
2.2 Homeostasis
Homeostasis is the maintenance of the body’s internal environment.
The internal environment of the body can be summed up in this following graphic:
Figure 2.12: Total Body Weight by Water Volume
The homeostatic conditions for homeostasis include the concentration of:
- Waste products
- Oxygen
- Nutrients
- Water
- Electrolytes
- Salts
- Temperature
- Pressure
- Volume
With that said, there are two different modes of regulating homeostasis: intrinsic (e.g., low O2 concentrations in muscles during intense exercise causes blood vessels to vasodilate) and extrinsic (done by the endocrine and nervous systems) control.
There are also three types of feedback in homeostasis that will be evaluated on in the following sections: negative (the most common), positive, and feed-forward.
2.2.1 Negative feedback
This happens when a change in one of the aforementioned homeostatic conditions triggers a response by the body that opposes the change (e.g., sweating on a hot and sunny day).
Negative feedback in an organism has the following five components:
- Sensations
- Afferent pathway
- Integrating center
- Efferent pathway
- Effector
2.2.2 Positive feedback
Here, a change in one of the homeostatic conditions causes a response by the body that accentuates the change.
A good example of this is childbirth in humans:
Figure 2.13: Child Birthing in Humans
2.2.3 Feedforward mechanism
Here, the body responds in anticipation of a change in one of the homeostatic conditions. An example of this would be insulin from the pancreas in anticipation of food.
2.3 The Integumentary System
2.3.1 Skin structures
The epidermis has an inner and an outer layer. The inner layer is comprised of rapidly dividing cells, whereas the outer layer is comprised of dead, flattened, and keratinized epithelial cells. The epidermis also contains: Granstein cells, Langerhans cells, keratinocytes, and melanocytes (which produces the skin pigment melanin).
The dermis is a layer of dense, irregular connective tissue rich in elastin and collagen fibers, nerve endings, and blood vessels.
The hypodermis is a loose layer of connective tissue where most of the body’s fat is stored.
2.3.2 Functions of the skin
The skin serves as a physical barrier between the outside and the inside environment (obviously). Furthermore, the skin has several roles in immune response:
Keratinocytes produce inflammatory cytokines and kill microbes.
Langerhans and Granstein cells are antigen-presenting cells.
The connective tissue in the hypodermis is also a site for immune responses.
2.4 Thermoregulation by the Skin
The body’s core temperature is constant and ranges from 36 to 37.5 degrees Celsius. The body’s skin temperature, however, changes depending on the environment’s temperature!
Interstingly, the body can withstand temperatures up to 43 degrees Celsius, but is more tolerant to cooling!
2.4.1 Heat loss mechanisms
The four heat loss mechanisms are:
- Convection
- Conduction
- Radiation
- Evaporation
2.4.2 Actions in Response to Changes in Temperature
In response to cold temperatures, the body may:
- Induce shivering
- Vasoconstrict blood vessels
- Cause behavioral adaptations
- Induce more brown fat activity
Alternatively, the body may perform the following when temperatures are high:
- Sweating
- Vasodilation of blood vessels
- Hypotonia (i.e., loss of muscle tone)
Figure 2.14: Fever Mechanism
Thermoregulation, when gone wrong, may result in the following:
- Hypothermia
- Hyperthermia
- Fever
2.4.2.1 What good does fever do to an organism?
When a pathogen is present in the host’s body, phagocytes engulf the pathogen and other leukocytes release inflammatory cytokines (e.g., TNF-alpha, IL-1, and IL-6). These cytokines then stimulate the anterior hypothalamus of the brain (i.e., the part of the body that regulates body temperature) to produce prostaglandin E2, hence leading to an increase in body heat production and increased vasconstriction (i.e., constriction of the blood vessels) - this leads to an increase in body heat.
Fever is a condition that increases the body’s temperature beyond its normal range. This is done by the hypothalamus to increase the optimal growth temperature for many microorganisms. Fever also leads to the production of heat shock proteins that are recognized by T-lymphocytes called delta gamma T-cells, hence resulting in the production of inflammation-promoting cytokines.
Higher body temperatures also increase the rate of enzymatic reactions in the body that increase the production and activity of phagocytes, speed up the multiplication of lymphocytes, and increase the rate of antibody production.
However, too high of a body temperature can denature the body’s enzymes. Hyperpyrexia is a fever with an extreme elevation of a body temperature greater than or equal to 41.5\(\omicron\)C. This is usually an indicator of an underlying, more serious condition.