2 Cervical Screening and intensive telephone-based case-finding
2.1 Methods
- Identify active eligible women who either have no recorded cervical screening or whose last recorded screening is very overdue (most recent result 45 months or older)
- One of two surveyors (Dr Buddini, or womens’ health nurse) will invite the woman to participate in cervical screening. The invitation will be done by telephone, using a telephone interpreter if required.
- If the invitation is accepted, an appointment is made for cervical screening.
2.2 Theory of Change
Figure 2.1: Theory of Change
2.3 Logical framework
| Objectives Hierarchy | Indicator | Verification | Assumptions/Threats |
|---|---|---|---|
| (Input) Invitation to cervical screening by telephone | Telephone invitation | Call log | Telephone answered |
| Common language used | |||
| Social desirability bias? e.g. type of practitioner ringing, or previous contact with practitioner who rings | |||
| Diqualifying criteria for cervical screening e.g. hysterectomy | |||
| (Input) Invitation to cervical screening by mail | Letter invitations | Previous letter in file | Letter read |
| English literacy | |||
| Letter persuasive | |||
| (Output) Appointment for cervical screening | Appointments made | Appointment log | Appropriate cervical screening already done elsewhere |
| Disqualifying criteria for cervical screening e.g. hysterectomy | |||
| Appointments attended | Appointment book | Appointment is remembered | |
| Cervical screening (CST) at clinic | Cervical screening results (can be searched using clinical database). | Some cervical screening will be the result of the telephone invitation, others might screen for other reasons. | |
| Cervical screening (CST) might be done elsewhere | |||
| (Outcome) Improved cervical screening coverage | Improved cervical screening coverage | Government Practice Incentive Program reports | |
| Increase detection of HPV or cervical changes | Patient record audit of HPV/ pLSIL/LSIL detected (Low-grade squamous intraepithelial lesion, possible or confirmed) | ||
| HSIL detected (High-grade squamous intraepithelial lesion) | |||
| (Impact) Reduce cervical cancer | Reduced cervical cancer rates | Difficult! | Vulnerable population screened |
2.4 Variables to measure
- Age
- Refugee or asylum seeker Possible proxy for less English literacy skills, or different health literacy.
- Interpreter usually required Usually recorded in clinical notes
- Patient seen by surveyor previously Could effect response rate
- Patient has had cervical screening before?
- Date of last recorded cervical screening
- Number of attempts to contact patient by telephone
- Patient contacted by telephone
- Interpreter used during telephone invitation?
- Patient had cervical screening done elsewhere appropriately?
- Patient ineligible for cervical screening e.g. has had hysterectomy
- Appointment made
- Appointment attended
- Cervical screening done at booked appointent as result of telephone invitation
- Cervical screening changes requiring review or referral
- Referral to gynaecologist as result of cervical screening
2.5 Population
Summary
## DOB Age SeenBuddini RefugeeOrAsylum
## Min. :1944-04-04 Min. :25.00 Mode :logical Mode :logical
## 1st Qu.:1954-05-04 1st Qu.:36.25 FALSE:200 FALSE:197
## Median :1969-06-20 Median :49.00 TRUE :90 TRUE :93
## Mean :1968-11-20 Mean :49.87
## 3rd Qu.:1982-03-08 3rd Qu.:64.00
## Max. :1994-02-27 Max. :74.00
##
## Subgroup AgeGroup5
## Buddini : 65 25 :40
## Refugee : 68 70 :38
## Refugee+Buddini: 25 45 :36
## Standard :132 65 :34
## 30 :26
## 60 :26
## (Other):902.5.1 Population overview
Number of patients at each age group, and whether they have a recorded refugee or asylum seeker background or seen by Dr Buddini in the past two years.
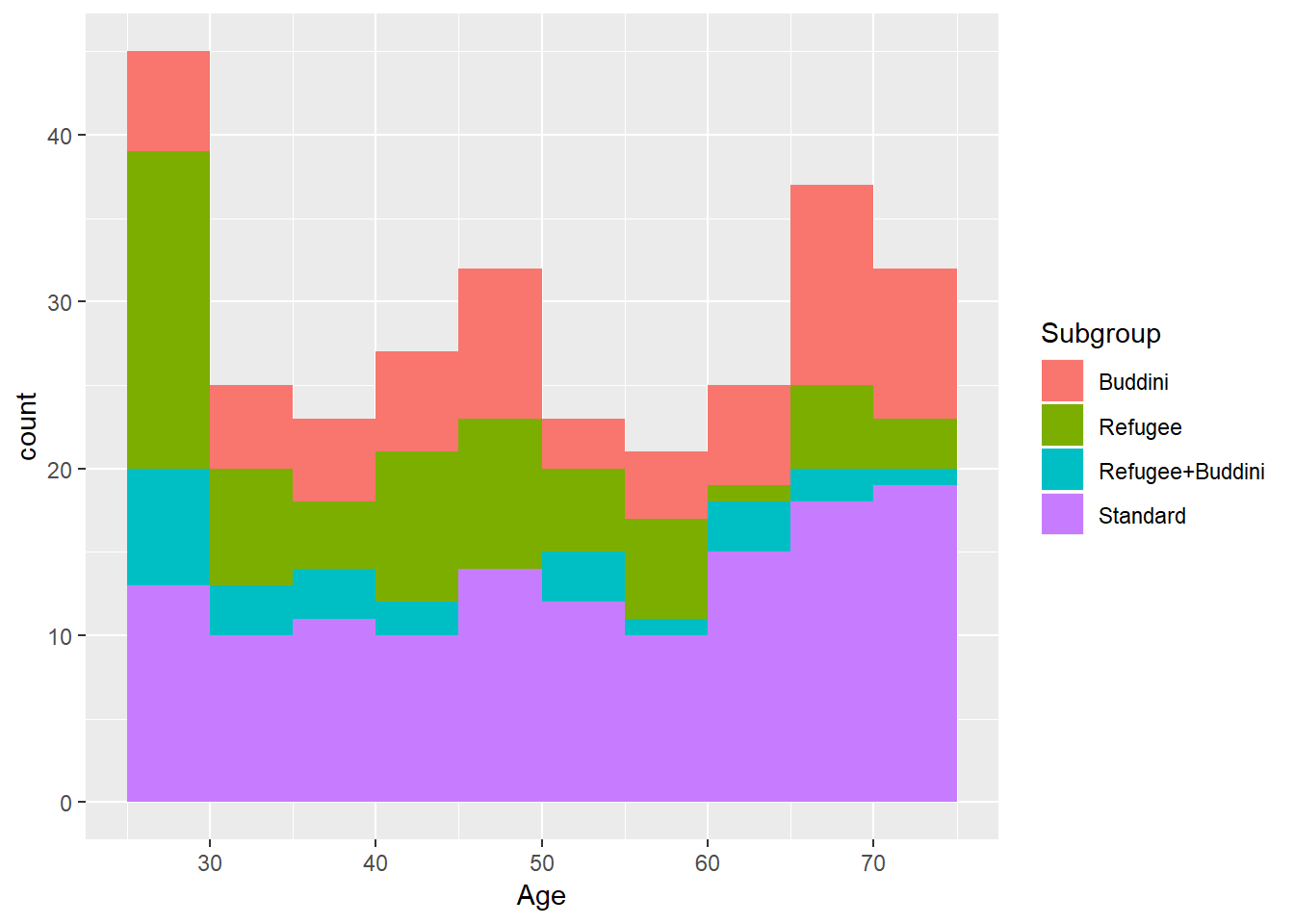
Figure 2.2: Population overview
Total population : 290
2.6 Power calculation
Previous proportion of under-screened patients who were screened in the three months after March 2018 was 5.2%. With a populaton of 290 patients, split between two groups, power of 0.8 and significance level of 0.05, the
##
## Two-sample comparison of proportions power calculation
##
## n = 145
## p1 = 0.05185
## p2 = 0.1507374
## sig.level = 0.05
## power = 0.8
## alternative = two.sided
##
## NOTE: n is number in *each* group## [1] "Minimum detectable effect : 0.0989"For further power calculation workings, including minimum detectable effect size at 6 months, see the Appendix - Power Calculation Details.
2.7 Phase 1 and Phase 2 group allocation
Complete randomization within sub-groups defined by age (5 years groups), of known refugee or asylum seeker background, and whether seen by Dr Buddini in the past two years.
Two surveyors were initially planned. One of whom was Dr Buddini. Each of the phase 1 and phase 2 were into two sub-groups for allocation to the surveyors.